Photo by cottonbro studio on Pexels.com
Your evening routine can affect your quality and quantity of sleep, regardless of what else is going on in your life. The activities you choose during evening hours may affect your capacity for falling asleep and staying asleep, and those can impact your mental wellness.
Poor-quality sleep, or lack of sleep, has many mental health consequences. If you don’t get enough restful sleep now, explore your evening habits and routines. You’ll be able to identify problem areas and then set up new routines that promote better sleep.
Try these 5 self-care habits to end your day and prepare for a night of restful sleep:
- Turn off the devices at the end of the day.
Do you find it hard to stop scrolling through your smartphone – especially social media accounts – before you try to fall asleep at night?
It’s too easy at bedtime to waste minutes – or hours – browsing cat memes and other non-important digital diversions. If your evening smartphone or tablet use is a problem, you can change the habits you have adopted.
Set limits on your use of technology as bedtime approaches. Turn off your computer, phone and tablet one to two hours before you’re ready to go to bed. Set an alarm if needed, to remind yourself.
- Set your bedtime ahead of time.
Your brain starts a winding down process before bedtime. It’s part of the natural awake-asleep cycle. Decide on a definite bedtime before that time. Try to stick to that bedtime every night, even on Saturdays and Sundays if you can. This consistent schedule trains your brain to feel tired naturally at bedtime.
- Plan ahead for the day tomorrow before bed.
Planning for tomorrow at 6 PM or so is an excellent way to get those things off your mind for the night ahead. Go over the calendar and check for meetings and appointments. Check your to-do list, prioritizing what you’ll need to get done.
Lastly, plan out what order everything tomorrow will be done in. You’ll be able to wake up in the morning to an organized schedule.
- Relax in a warm bath before you go to bed.
As a part of your natural wake-sleep cycle, your body goes through changes during the day. Melatonin production is part of that cycle. It starts in the evening and is accompanied by your core body temperature dropping.
A warm bath can help by triggering a similar sleepy reaction. Relax in your tub for an hour or more before bedtime. The water heats your body, then it will quickly cool down as the water is evaporating. This creates a sensation to make you relaxed and tired.
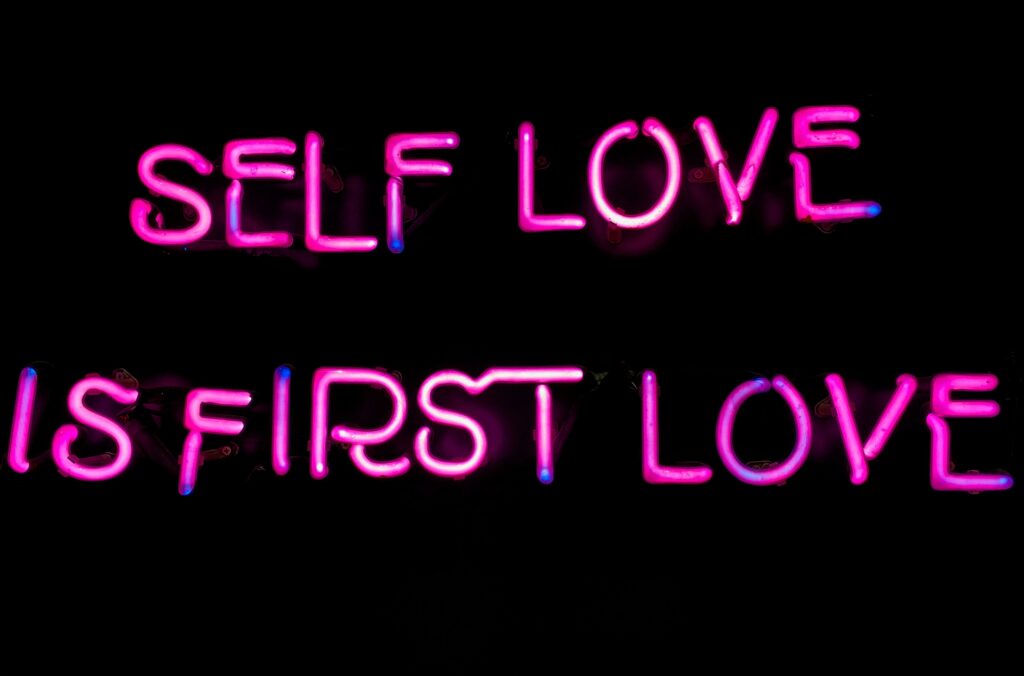
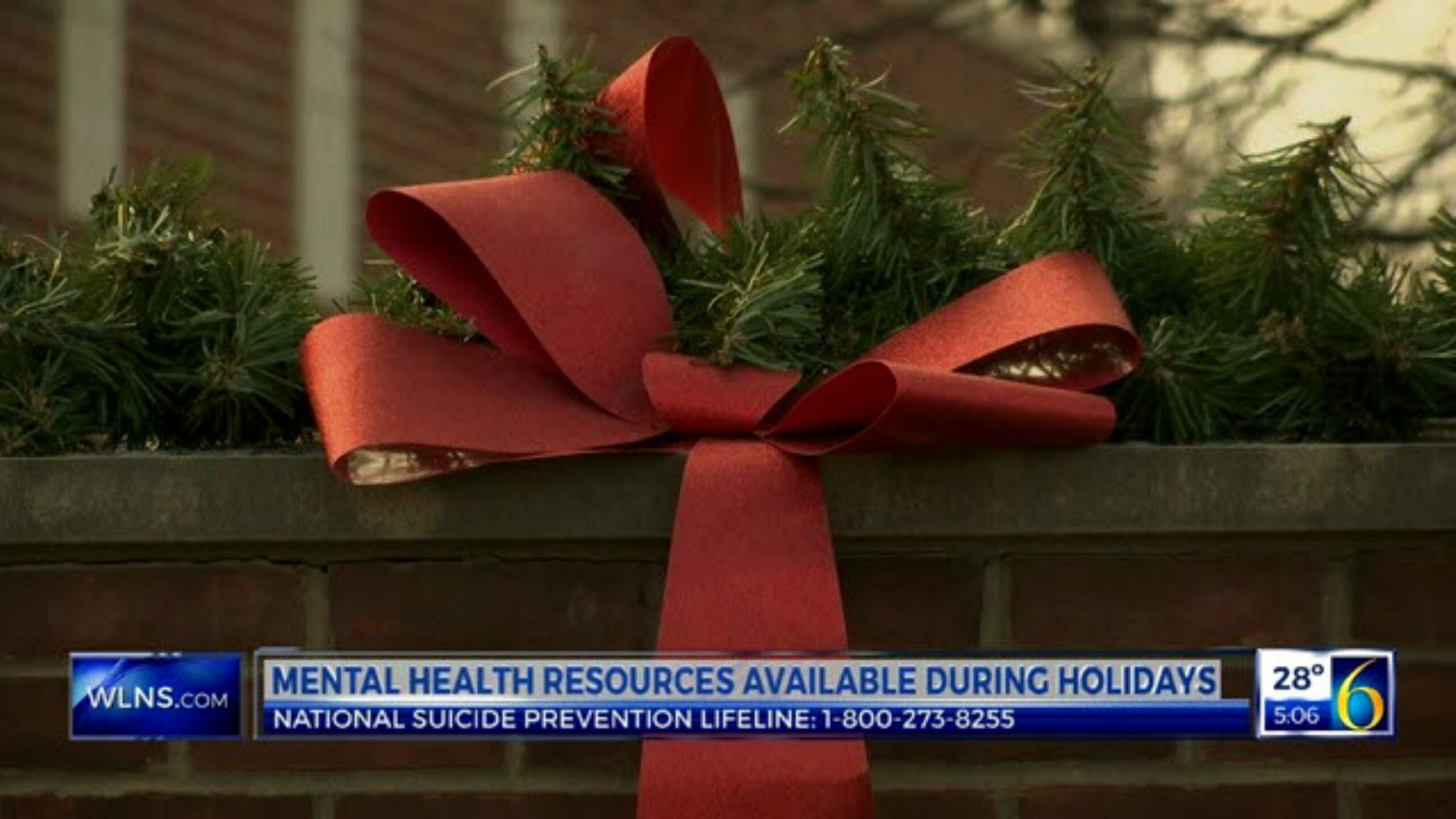
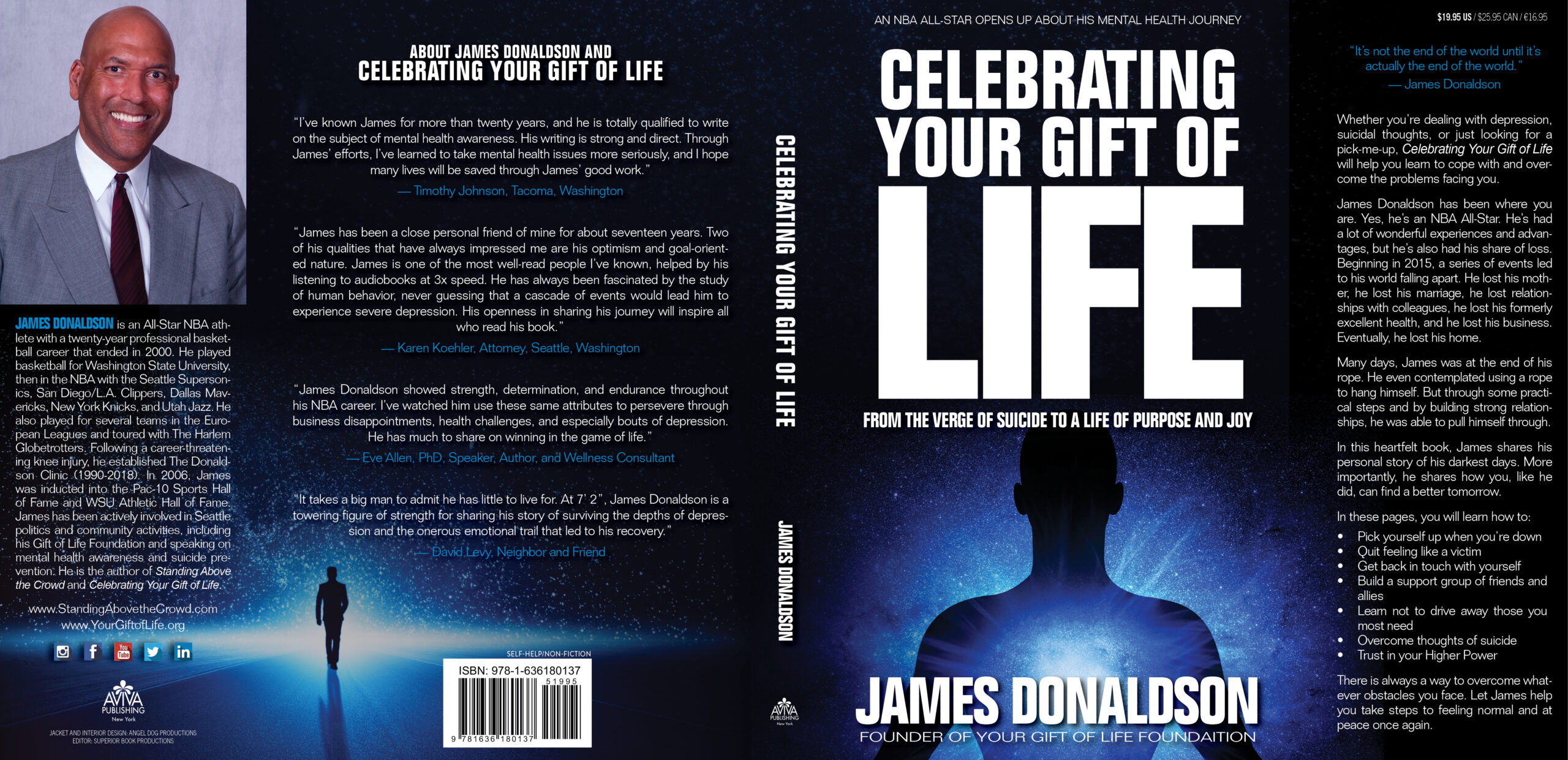
#James Donaldson notes:Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticleFind out more about the work I do on my 501c3 non-profit foundationwebsite www.yourgiftoflife.org Order your copy of James Donaldson's latest book,#CelebratingYourGiftofLife: From The Verge of Suicide to a Life of Purpose and Joy
www.celebratingyourgiftoflife.com
Link for 40 Habits Signupbit.ly/40HabitsofMentalHealth
If you'd like to follow and receive my daily blog in to your inbox, just click on it with Follow It. Here's the link https://follow.it/james-donaldson-s-standing-above-the-crowd-s-blog-a-view-from-above-on-things-that-make-the-world-go-round?action=followPub
- Spend a bit of time meditating before ending your day.
Starting and ending your days with sessions of meditation can be helpful in getting geared up for the day and then winding down for the night.
Let your thoughts arrive as they will and observe them. Connect with your body’s sensations. Observe any thoughts related to whatever happened in your day. Then let go of them, to help you lose the attachment to any energetic feelings about the day.
Conclusion
Evening routines may be different for everyone, but most will have the same basic ideas – putting the day behind you, preparing for the next day and then unwinding into restful sleep. The routines are quite flexible and include things you love as well as things that must be remembered.
Your routine in the evening defines what you’ll be doing tomorrow, as well as what you did today. You want to spend the last couple hours before bedtime using self-care techniques that end your day the right way, with a restful night ahead. This is most beneficial for mental wellness.
Photo by cottonbro studio on Pexels.com https://standingabovethecrowd.com/james-donaldson-on-mental-health-evening-routines-for-mental-wellness-5-self-care-habits-to-end-your-day-right/




 Veterans salute Nov. 11 as the national anthem is played at the Veterans Day ceremony at the Oklahoma National Guard Museum.
Veterans salute Nov. 11 as the national anthem is played at the Veterans Day ceremony at the Oklahoma National Guard Museum.