James Donaldson on Mental Health - 6 Reasons Men Don’t Get Mental Health Care When They Need It
4 ways to help men's mental health

Reviewed by Hara Estroff Marano
KEY POINTS
- Depression can present differently in men, which means it might get missed.
- Stigma and beliefs about masculinity can deter men from seeking the care they need.
- Listening, creating a safe place, and recognizing struggles are steps to helping resolve barriers for men.
By Bryant Clayton, Psy.D., and John Rucker, Psy.D.
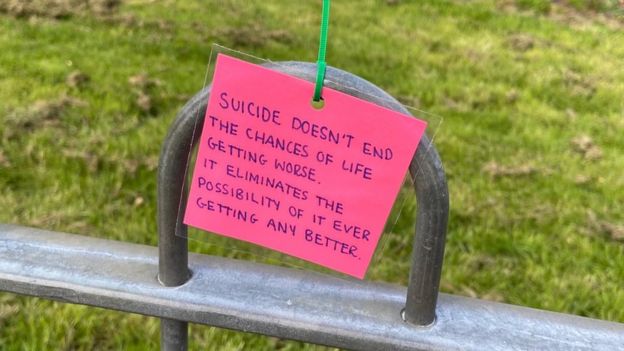
Men face an inordinate difficulty seeking and accessing mental healthcare. In the U. S. alone, six million men are affected by depression each year, with some dying by suicide at a rate four times higher than women. In fact, men’s rates of suicide are greater than women across all ages and most of the lifespan.
And yet, an official diagnosis of depression in men is half that of women. Some contend this does not suggest the absence of depression in men but, rather, that 1) men are less likely to present for care and thus less likely to receive a diagnosis, and 2) that men’s depression presents differently (male depressive syndrome), such as with greater anger, alcohol misuse, risk-taking, tiredness, irritability, and claiming to be “on autopilot.”
In addition, men appear two and a half times more likely to die of alcohol-related causes than women. Men are also two to three times more likely to misuse drugs than women.
Several barriers impede men’s willingness to seek and benefit from mental healthcare. These barriers are concerning, considering the alarming and increasing epidemics of suicide, substance use, and problematic coping styles among men (Seidler et al., 2016; Bilsker et al., 2018; Seidler et al., 2019).
#James Donaldson notes:
Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.
Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.
Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticle
Find out more about the work I do on my 501c3 non-profit foundation
website www.yourgiftoflife.org Order your copy of James Donaldson's latest book,
#CelebratingYourGiftofLife: From The Verge of Suicide to a Life of Purpose and Joy
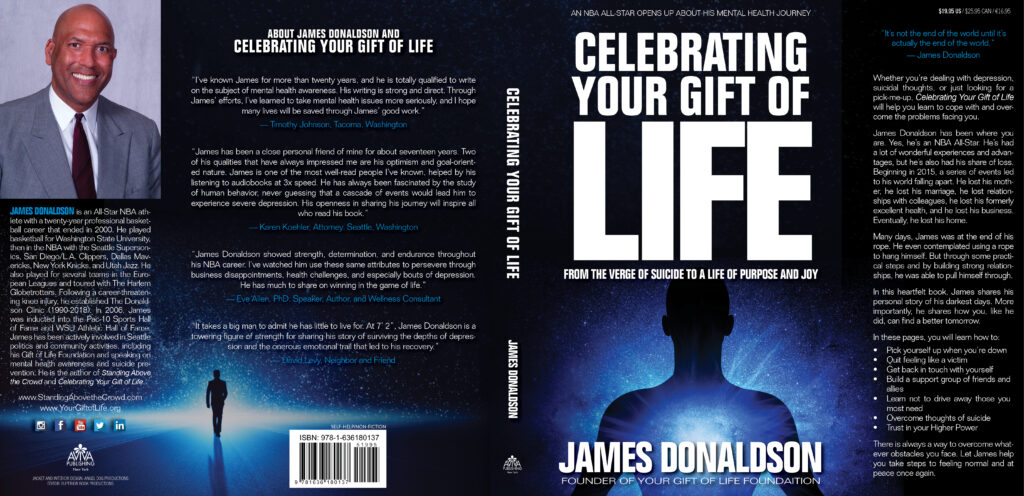
www.celebratingyourgiftoflife.com
Link for 40 Habits Signup
bit.ly/40HabitsofMentalHealth
If you'd like to follow and receive my daily blog in to your inbox, just click on it with Follow It. Here's the link https://follow.it/james-donaldson-s-standing-above-the-crowd-s-blog-a-view-from-above-on-things-that-make-the-world-go-round?action=followPub
Barriers Men Face to Seeking Help
- Dominant masculine ideals, often involving stoicism, independence, strength, and control
- Poor mental health knowledge, which can manifest as difficulty communicating or recognizing a need for psychological help
- Societal and self-stigma, which can cause shame about being seen as weak, discomfort with emotional disclosure, and problem minimization
- Atypical symptom expression (male depressive syndrome), which isn’t adequately captured in current diagnostic criteria
- Clinician biases, stereotypes, and discomfort due to rigid assumptions regarding common male behaviors and responses
- Lack of men-centered services.
Montgomery et al. (2011) advocated a need for men-centered care after finding that fathers with mental health concerns and troublesome social conditions had poorer health outcomes. A decade later, Vassallo et al. (2021) concluded similarly after gender-sensitized strategies for men successfully reduced problematic masculine messages of self-reliance and interpersonal dominance.
Multicultural Factors in Men’s Mental Health
Men from minority communities may experience additional sociocultural barriers that further decrease the likelihood of seeking mental health services. At times, men from minority communities could be expected to develop their own solutions when expressing problems to loved ones, lest they jeopardize security and respect in their family unit or roles of authority, work, and leisure. This can hinder their capacity to communicate thoughts, emotions, and bodily disturbances in a healthy, constructive way.
Other relevant sociocultural factors men in marginalized groups face include stigma from their culture of origin, mistrust in public health authority due to histories of systemic discrimination and/or racism, spiritual/religious barriers whereby mental health disorders are conflated with exclusively spiritual concerns, narrow masculine ideals/standards (i.e., machismo in Latin American culture; mental illness as weakness in some Asian communities), and believing their voice or perspective does not matter.
Four Strategies to Support a Man’s Mental Health
- Lend an ear. Recognized that your interactions with the men in your life matter. Your willingness to listen, understand, and dedicate space for men to be vulnerable, mess up, and learn are integral to helping them develop, cope, and become better fathers, husbands, leaders, workers, and citizens of the world.
- Recognize effort with thoughtful affirmation and recognition. We all long to be appreciated. Men often do not feel appreciated unless they are sacrificing and suffering for the sake of others, especially those closest to them. Be willing to recognize and verbalize good efforts, psychological growth, and positive qualities in the men in your life. Encourage them. Limit unnecessary criticism.
- Collaborate to solve problems. When you lend ears and give recognition, you may better empathize and understand the mind/perspective of the person. While this may not eliminate identified concerns, it may facilitate a united front against psychological troubles. In addition, a collaborative spirit can decrease loneliness and boost self-confidence and esteem.
- Get more minds on the case. If a man in your life is troubled by things that go beyond your capacity to help, you might honor the importance of his health by seeking professional guidance. Having “more minds” on a case can bring forth new ideas, fresh perspectives, and innovative solutions to managing life’s problems.
The road to more effective and accessible mental healthcare for men is worth traveling. A dedicated month to honor men’s mental health is a step towards awareness and inclusivity. And yet, mental health knows no calendar. Continuing to elicit discussion with men about their mental health in a nonjudgmental, curious way should be a year-round mission, and more important, an everyday task.

https://standingabovethecrowd.com/james-donaldson-on-mental-health-6-reasons-men-dont-get-mental-health-care-when-they-need-it/