Photo by Pixabay on Pexels.com
Photo by Pixabay on Pexels.comJarrid Wilson, Darrin Patrick, Andrew Stoecklein, Isaac Hunter, Ed Montgomery, David Treadway, Teddy Parker Jr. Some of these names may sound familiar to you. That’s because they made the news as pastors who have died by suicide. The death of anyone by suicide is shocking and heartbreaking. But when it’s a pastor—a spiritual leader—the aftermath is even more devastating.
Jarrid Wilson was an associate pastor at Harvest Christian Fellowship in Riverside, California. He was a mental health advocate and spoke openly about related issues. On the morning of September 10, 2019, Wilson tweeted:
“Loving Jesus doesn’t always cure suicidal thoughts. Loving Jesus doesn’t always cure depression. Loving Jesus doesn’t always cure PTSD. Loving Jesus doesn’t always cure anxiety. But that doesn’t mean Jesus doesn’t offer us companionship and comfort. He ALWAYS does that.”
“He’s in hell, man.” “Did have the Holy Spirit?”
Later that night, Jarrid Wilson ended his life. Many responded to the news online, questioning Wilson’s faith and his decision to take his life. These are just a handful of tweets and Facebook comments:
“When you are full of Christ, there will be no room for depression or frustration. The fullness of Christ in you will choke it out.”
“Truly, Jesus could have delivered you from all those afflictions but you decided not to let Him take control of your situation and rather you focus on what your human eye saw. Now you have many believing this
. . . not true!”
“He’s in hell, man.”
“Did have the Holy Spirit?”
Not every response was like this. Some offered sincere condolences to Wilson’s family, shared their fondest memories and thanked him for how he had helped others overcome difficulties. But when Jarrid Wilson took his own life, it sparked a discussion online in comment sections and opinion pieces alike. At the root of many of these conversations were people trying to reconcile Wilson’s faith in God with his final action. Was there truth to the sentiment that he just didn’t love God enough?
is faith enough?
Jesus spoke quite radically about the power of prayer. He said, “Whatever you ask for in prayer, believe that you have received it, and it will be yours” (Mark 11:24). He even went so far as to say that if you have faith with no doubt, your faith can move mountains (Matthew 17:20). So it’s understandable that Christians would apply this logic to mental health struggles. Surely if the afflicted prays fervently enough and has faith, God could cure their mental illness.
It’s important to note the biblical authors don’t write about mental illness in the same way we talk about it today. But they do frequently mention times people had been struck down by physical illness: lepers, a woman who bled for 12 years, paraplegics and more. If you’ve read the stories, you’ll know Jesus healed many of these people because of their faith in Him.
In the case of the woman who bled for 12 years, this is what Matthew, a disciple of Jesus, said of her affliction: “A woman who had been subject to bleeding for 12 years came up behind him and touched the edge of his cloak. She said to herself, ‘If I only touch his cloak, I will be healed.’ Jesus turned and saw her. ‘Take heart, daughter,’ he said, ‘your faith has healed you.’ And the woman was healed at that moment” (Matthew 9:20–22).
This is one of many examples of how someone was healed because of their belief that Jesus was capable of healing them.
modern miracles still happen
God’s healing hand is not limited to the stories in the Bible. I have met people who are walking miracles—people who have defied a doctor’s prognosis that “they should be dead”. I know these people had committed Christians all around the world praying for their recovery. And recover they did.
But I have also met people who lost loved ones despite the committed Christians who prayed “without ceasing”. I’ve heard stories of people’s faith being shattered because they truly believed God would save their loved ones—and yet death still took them. I won’t pretend to understand why God intervenes on behalf of some and not others. It’s something I have brought to Him in prayer many times myself. What I can offer is a little perspective. A believer’s heartfelt prayers may not have saved their life on Earth, but we believe that by God’s grace we will see them again. Death is never easy. But for Christians, this is when the promise of what comes after death comes in. In the end, what really matters is where that person sits with God. As a follower of Jesus, I have hope that death is not the end and I will see my loved ones again one day—in a world free from death and suffering.
Death is never easy. But for Christians, this is when the promise of what comes after death comes in.
Just like physical health, there are things you can do to improve your mental health: healthy eating, moving your body, adequate sleep and rest. And from a spiritual point of view, spending time in prayer and immersing ourselves in God’s Word can also be beneficial. But sometimes—like when treating broken bones or cancer—a healthy lifestyle isn’t enough. Just like Christians fighting cancer may pray as part of their treatment, most also seek out medical support.
what about me?
Ellen White was a prolific author and co-founder of the Seventh-day Adventist Church, as well as an advocate for healthy living. She encouraged Adventists to open healthcare facilities,1 recognizing the importance of medical treatment when natural preventatives fail. She saw that God has equipped humans with incredible bodies that, if treated well, treat us well. But she also saw that God has given us the gift of medical knowledge and that there is wisdom in combining healthy habits with medical treatment. This logic also applies to mental health.
At my lowest, I wished that I could cease to exist
This topic is especially close to my heart. I was 21 years old when my mental health hit rock bottom. At my lowest, I wished that I could cease to exist. I never fell so deep into my depression that I tried to follow through on that desire, but I can certainly see how someone could.
It’s important to note that mental illnesses, like depression, are not always cured with practicing gratitude, eating well or having a healthy relationship with God. While mental illness can be caused by external pressures like trauma, stress, substance abuse and environmental factors, it can also be caused by biological factors such as genes, brain chemistry or hormonal imbalances.2 When healthy habits aren’t enough to squash dark thoughts, the next step is often medical treatment. Therapy, medication or both may be prescribed to treat mental illness.
What pulled me from my dark pit was a combination of treatments. I vividly remember leaning into my faith, clinging to the Psalms and certain promises God makes to His people, and finding a sense of peace and relief from those passages. But I also paired this with practical steps to help improve my wellbeing. I removed study stressors by doing a semester of university via distance so I could live at home with the support of my family. I started seeing a psychologist and made good progress with her. But it soon became clear I needed additional support and so I began to take anti-depressants.
After a few months, color returned to my life. I would make it a day without crying, then two and then my life returned to the usual ups and down one can expect when their world isn’t tainted by depression.
I would make it a day without crying, then two and then my life returned to the usual ups and down one can expect when their world isn’t tainted by depression
#James Donaldson notes:
Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.
Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.
Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticle
Find out more about the work I do on my 501c3 non-profit foundation
website www.yourgiftoflife.org Order your copy of James Donaldson's latest book,
#CelebratingYourGiftofLife: From The Verge of Suicide to a Life of Purpose and Joy
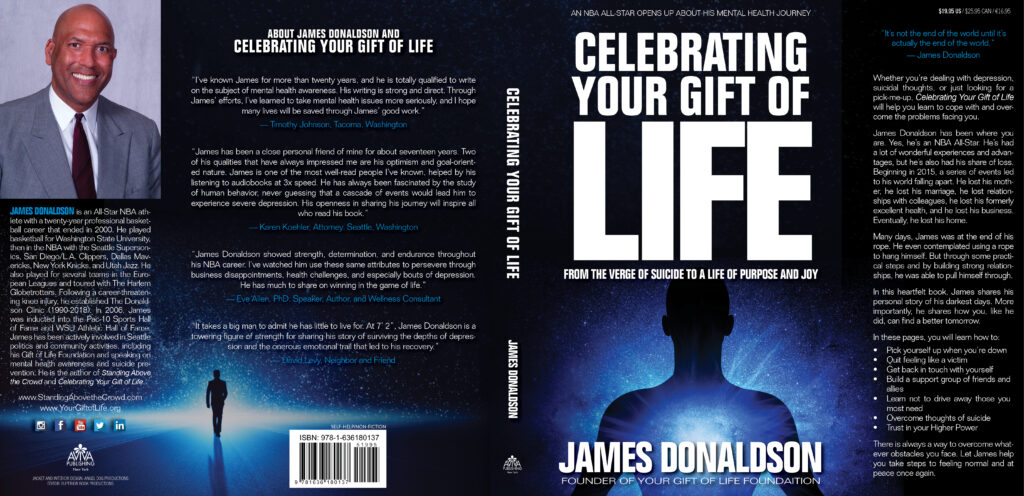
www.celebratingyourgiftoflife.com
Link for 40 Habits Signup
bit.ly/40HabitsofMentalHealth
If you'd like to follow and receive my daily blog in to your inbox, just click on it with Follow It. Here's the link https://follow.it/james-donaldson-s-standing-above-the-crowd-s-blog-a-view-from-above-on-things-that-make-the-world-go-round?action=followPub
For someone who has never experienced poor mental health, a journey like mine is almost impossible to grasp. Most people are shocked when they learn of my mental health struggles because, from all they see, I have a sunny disposition. But it is not as straightforward as choosing to be happy. Trust me, no-one feeling those levels of despair would choose to feel that way if feeling happy was an option. Mental illness is a health condition that needs treatment in the same way that physical illness needs treatment. And just like physical illness, mental health treatment will look different for everyone.
So, back to Jarrid Wilson. How does faith in God intersect with suffering from ? The replies to Jarrid’s tweet imply that if he truly loved God, he would still be here—that he just needed to try harder.
I believe those replies missed the point entirely. Mental illness is just another part of a world filled with suffering. Rather than judging each other and arguing in the comments section, we should be supporting one another through the tough times of life. Every person is precious to God. And if being a listening ear or a helping hand in a time of need can save someone’s life on Earth, then it’s something all of us should be striving towards.
 Photo by Pixabay on Pexels.com
Photo by Pixabay on Pexels.com https://standingabovethecrowd.com/james-donaldson-on-mental-health-what-does-the-bible-teach-about-mental-health-and-suicide/