Some hold it together at school, only to lose it at home. Others stress out in the classroom.

Writer: Beth Arky
Clinical Experts: Stephanie A. Lee, PsyD , Jerry Bubrick, PhD
What You'll Learn
- Why do some children act out at school but not at home?
- Why are some kids better behaved at school than at home?
- What can parents do to help kids behave better and feel better?
-
Quick Read-
Full Article-
Why do some kids do better at school?-
Suppressing symptoms at school-
Why do some kids do better at home?-
How to help kids-
Therapies that can helpSome children seem very different at home and at school. That can be confusing to parents and make you wonder if you’re doing something wrong.
Some kids with learning or behavior issues do great at school, where structure makes them feel secure. At home, though, they totally lose it. For other kids, the opposite is true. School triggers their symptoms because it is stressful for them. They seem like different kids at home, where they’re more relaxed.
There are also kids who work so hard to keep it together at school that they melt down the second they get home. That’s because parents may not be as strict and will love them no matter what. These kids include some with autism, OCD, anxiety or ADHD.
To understand what your child’s behavior might mean, the first thing to do is talk to the teacher and compare notes. This helps you both figure out what’s causing stress for the child and what’s causing the behavior. Then you can work on ways to help your child feel better, which helps with behavior.
For kids who do better at school, adding more routine and structure at home can help. If the change from school to home is hard, then downtime and a snack can help. It goes the other way too. If parents have routines that help kids at home, then sharing those with the teacher can help kids at school.
For kids who need more help with behavior, the best treatment is called cognitive behavioral therapy (CBT). CBT teaches kids how to manage their emotions when they get too big and strategies to control their behavior. And parents also get trained in how to help their kids.
It’s not unusual for kids to behave differently in different settings. For instance, you’d expect a child to act one way at a friend’s birthday party and another at her grandparents’ house. But the behavior of some kids — especially those with issues such as anxiety, learning disabilities, ADHD and autism — can vary much more markedly, especially when they’re at home versus school. This discrepancy can leave parents puzzled, if not upset, and worried that they’re doing something wrong.
#James Donaldson notes:
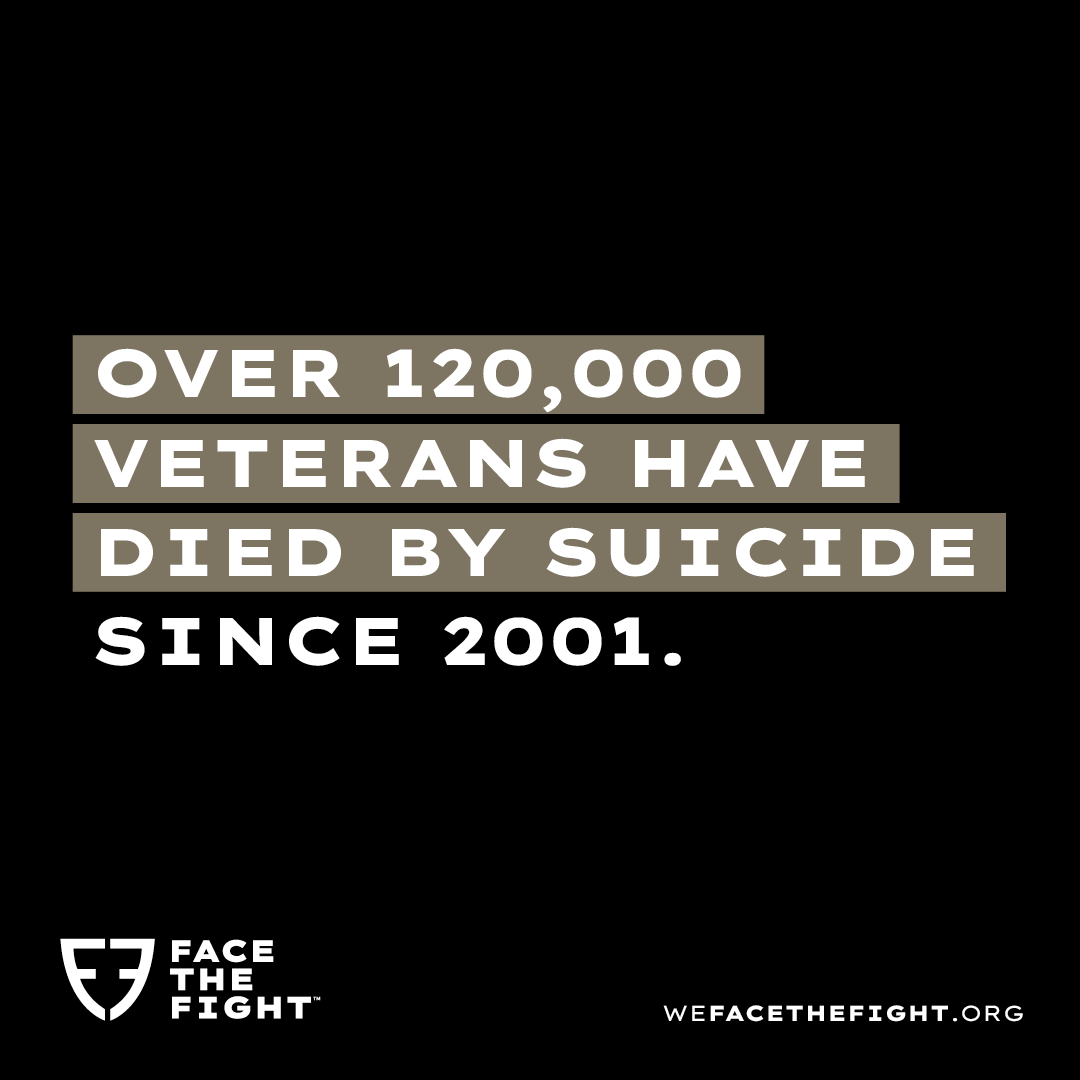
Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.
Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.
Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticle
Find out more about the work I do on my 501c3 non-profit foundation
website www.yourgiftoflife.org Order your copy of James Donaldson's latest book,
#CelebratingYourGiftofLife: From The Verge of Suicide to a Life of Purpose and Joy
Click Here For More Information About James Donaldson
Take the case of Sam, now 15, who is gifted but also diagnosed with autism spectrum disorder, ADHD and learning challenges. His mother, Maratea Cantarella, who serves as executive director of Twice Exceptional Children’s Advocacy, recalls how challenges at school led to explosive behavior at home.
At school, between trying to please his teachers and interact with peers, “he was really working hard to keep himself in control,” Cantarella says. By the time he got home, “I felt often that he was just looking for a way to release all the built-up tension.” Release it he did, with 30-minute tantrums over homework or “really anything.” Afterward, when he was calm, she adds, “he would feel terrible shame and guilt.”
But for some kids, school is where their challenges are most visible. Chloe, 8, has selective mutism and social anxiety. Her mother, Kim Byman, says that at home, Chloe is a “fun, goofy, talkative, energetic girl.” But when she gets to school, she shuts down. She has never spoken to her teachers or classmates, though she participates in all areas that don’t require being verbal. She won’t ask to use the restroom; she waits until she gets home.
So why is it kids can perform so differently in different settings?
Why do some kids do better at school?
Some children may do a good job meeting expectations at school, but it’s such a struggle for them it will take its toll at home. Children with ADHD, anxiety, autism and learning disabilities “may be using a lot of their resources to follow directions or cope in the classroom,” says Stephanie Lee, PsyD, a clinical psychologist. Once all these kids get home, “it’s challenging for them to conjure up the same amount of resources to manage.”
Meanwhile, she adds, many kids, including those on the autism spectrum, benefit from the consistency, structure, predictability and routine that come with their school environment. This often cannot be mirrored at home “because that’s not how life works,” she says.
At school, rewards and consequences are likely to occur in a consistent way that may be more challenging for parents to set up at home. Also, social modeling in school can help kids fall into line, literally and figuratively. Finally, teachers have no time for dawdling: If a child doesn’t follow a direction on the first or second prompt, the teacher will likely have an immediate consequence, whereas parents might end up allowing their child to avoid or delay the next step because they spend a lot of time talking about it.
Suppressing symptoms at school
Jerry Bubrick, PhD, a clinical psychologist who treated many children with anxiety and OCD at the Child Mind Institute, notes that kids with some disorders, including anxiety and OCD, are very concerned about how people perceive them, especially when they get into the middle and high school years. So they really try to hide their symptoms. “Typically, we’ll see kids functioning at a higher level at school,” says Dr. Bubrick, “less symptomatic because they’re trying to maintain this social perception that they’re fine. And they tend to have a lot of embarrassment and shame around their symptoms.”
Another key reason kids do better at school: They feel safe to be “their worst selves” at home, secure in the knowledge that their parents will still love and support them.
“I think sometimes kids come home and it’s like when you take off your shoes and feel a sense of relief,” Dr. Bubrick explains. “Like, ‘OK, I can be myself now.’” For kids who have done a really good job of suppressing their symptoms at school, at home, where they feel there’s no one judging them, “there can be an explosion of symptoms.”
As one mom of a 10-year-old with OCD recalls, at school her daughter would rock herself or doodle on a sticky pad to resist her obsessive thoughts, even though she was in distress. “So she would bottle it up at school, and then basically come off the bus at home and just explode,” she says. “Physically and verbally, she was very upset.”
This, too, can leave parents confused. “It’s common for parents to say, ‘I go to the school and the teachers say, Johnny is so lovely in class and I don’t see him squirming. I don’t see any of these things that you’re talking about,’” Dr. Bubrick says. “And then the kid comes home from school and he’s really symptomatic and having a hard time controlling it.”
Why do some kids do better at home?
For most kids, academic and social demands at school are above and beyond what they typically face at home, notes Dr. Lee. That may trigger problem behaviors in some their families never see at home.
Kids with challenges like ADHD and anxiety often have a very low frustration tolerance; asking them to be patient or persistent at school can be a big stressor. “That can be incredibly challenging for kids,” Dr. Lee says, “so we might see a lot of acting out in those types of situations.”
Similarly, children with social anxiety who have worries about how they’re being perceived by others, or children who have anxieties relating to performance, might not have any problem behaviors at home. But when they get to school and have to do math or read a passage aloud, they might engage in some negative behaviors to avoid that. “Acting out in this particular situation might end up being functional for them,” Dr. Lee says, “because if they act a little silly, the teacher might scold them, but then they move on.’”
When it comes to autistic kids, they may be allowed very ritualized or self-directed behavior at home, such as screen time or Legos. When they get to school, not being allowed to do those things, or having to wait for activities they may have free access to at home, can be very challenging for them. This can also lead to disruptive behavior.
How to help kids
One of Dr. Lee’s major suggestions is encouraging collaboration and open communication between home and school as much as possible. “If there are strategies or techniques that the child is really benefiting from at home or in school, can they be shared and adapted to support that child in both environments?” she says.
For instance, she notes, if a child is helped by being able to see a visual schedule in school, can one be created for home? “Similarly,” she adds, “if we know that a child really benefits from when/then statements at home — meaning ‘when you do this, then this will happen’ — share that with the teacher.”
Dr. Lee says the best way to create a collaborative relationship with the school is to “make sure you praise the teacher and value the work they’re doing in addition to giving them information about your child.”
For kids whose problem behavior comes out at home, Dr. Lee recommends that they get a chance to decompress when they transition after school: “It’s absolutely OK to have less stringent demands during that period of time for your child if they need a break. That said, it’s important for them to understand that the rules of the household still need to be followed.”
Dr. Bubrick echoes that idea, saying it’s vital to note how well-nourished and well-rested the child is. Coming home starving, after struggling all day to keep it together, is a good recipe for an afternoon meltdown. He advises parents to get kids back on track by giving them a snack and having them rest, allowing them to regroup to get a healthy start for the evening.
Therapies that can help
The tool most experts recommend to help kids manage their behavior, whether at school or at home, is cognitive behavioral therapy, or CBT. CBT has been adapted for many different kinds of emotional and behavioral challenges; what these specialized therapies all have in common is that kids learn self-regulation skills, or how to handle powerful emotions in better ways than acting out impulsively.
When kids use CBT skills at school, they are able to function better without having to expend so much energy, Dr. Bubrick explains. So when they get home, there’s less stress and the possibility of an explosion of symptoms. “The more kids practice these skills,” he says, “the better they get at them.”
Dr. Bubrick notes that with CBT, parents are included from the beginning, to understand their child’s condition and see what things they’re doing that are, despite good intentions, contributing to the problem. “We teach parents the dos and don’ts on how to parent a child with anxiety disorder,” he says. He gives the example of a child with OCD who is afraid of germs. A parent doesn’t do the child any favors by opening doors for him. Instead, the child must learn skills that will help him deal with his anxieties and compulsions.
Dr. Lee says behavioral parent training, which includes components of CBT, is often what is needed to assist parents in determining what’s going on in either environment and the best way to support their child.
 https://standingabovethecrowd.com/james-donaldson-on-mental-health-why-are-kids-different-at-home-and-at-school/
https://standingabovethecrowd.com/james-donaldson-on-mental-health-why-are-kids-different-at-home-and-at-school/