By David Smith, CCP, RN, BSN, CFRN, CEN, FPC
Introduction: The Hidden Toll of the Job
You pull into the station after a grueling 24-hour shift. The cardiac arrest on scene turned into a dead on arrival. The child with the head injury wasn’t breathing when you arrived. Your last patient coded twice on the way to the emergency room (ER).
Now, as you sit in your car before heading home, you feel numb.
Emergency medical services (EMS) providers are trained to save lives, endure trauma, and push through exhaustion. But what happens when the weight of the job becomes too much?
The statistics are staggering:
- 37% of EMS providers meet the clinical criteria for post-traumatic stress disorder (PTSD), compared to 6% of the general population.1
- Depression and anxiety rates in EMS are 5–10 times higher than in other professions.2
- EMS providers are 1.39 times more likely to die by suicide than the general population.3
Yet, mental health in EMS remains heavily stigmatized, forcing providers to suffer in silence.
The Reality of EMS Mental Health: What We’re Not Talking About
The stressors of EMS are relentless and cumulative. Unlike hospital-based clinicians, EMS personnel operate in unpredictable environments, with little control over what comes next.
1. The Accumulation of Trauma: PTSD in EMS
Daily, EMS providers encounter death, violence and suffering. Over time, these experiences re-wire the brain, leading to:
- Hypervigilance – Constant alertness, even off duty.
- Flashbacks & intrusive thoughts – Reliving traumatic calls.
- Emotional numbness – Struggles connecting with family and friends.
A 2020 study found that first responders process trauma similarly to combat veterans, yet many do not seek help due to fear of judgment or job repercussions.4
2. The Burden of Depression and Anxiety
- Long shifts, sleep deprivation, and workplace stress contribute to high rates of chronic depression in EMS.
- Anxiety and panic attacks are frequently reported but often go untreated.
- EMS providers with untreated depression are more likely to make critical medical errors on scene.5
3. The Suicide Epidemic in EMS
The harshest reality?
- EMS providers are at higher risk of suicide than firefighters, police officers, and even military personnel.3
- Many turn to substance use, alcohol, or isolation rather than professional support.
We are losing our own, and the system is doing little to stop it.
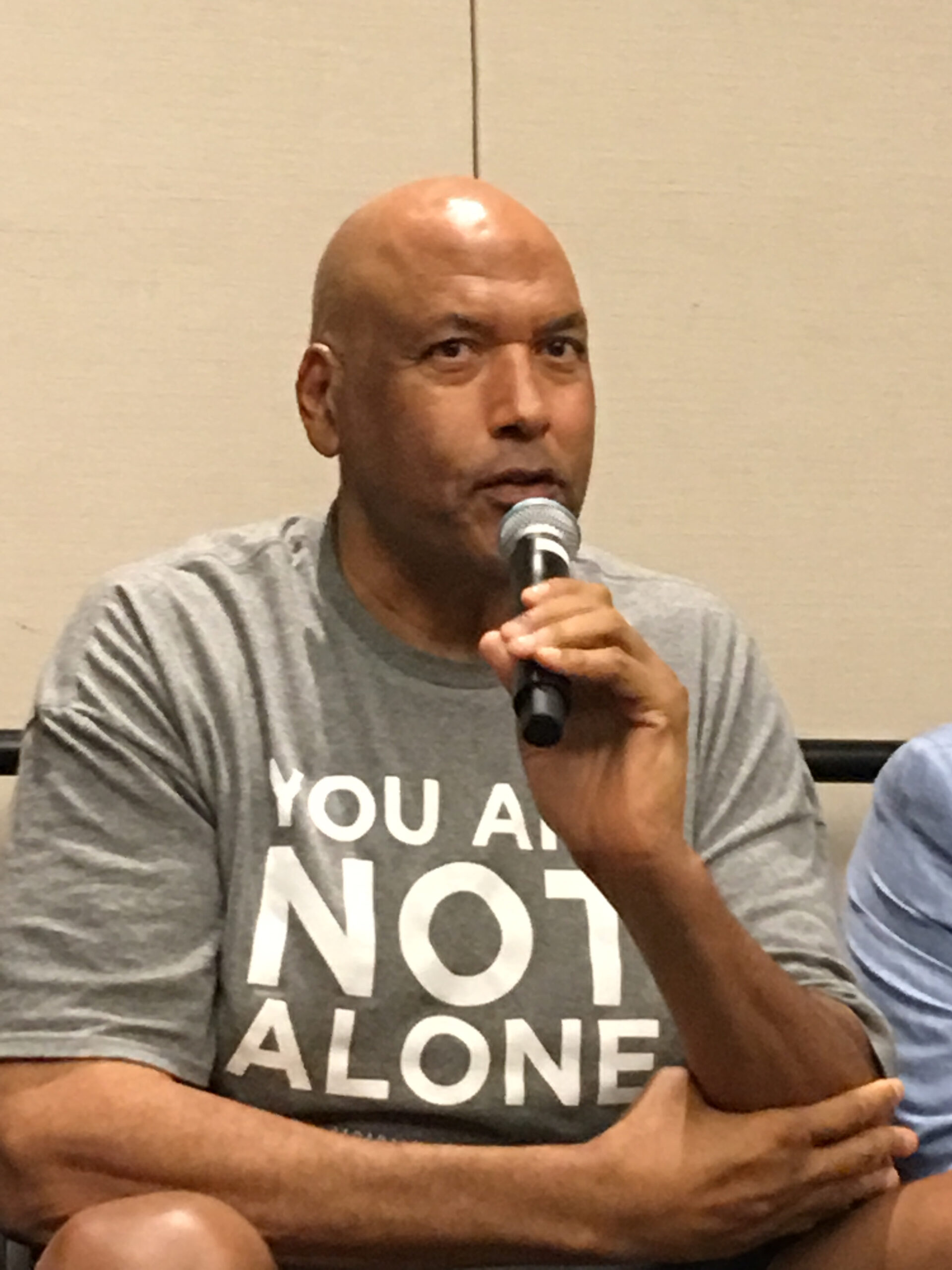
#James Donaldson notes:
Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.
Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.
Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticle
Find out more about the work I do on my 501c3 non-profit foundation
website www.yourgiftoflife.org Order your copy of James Donaldson's latest book,
#CelebratingYourGiftofLife: From The Verge of Suicide to a Life of Purpose and Joy
Click Here For More Information About James Donaldson
Breaking the Stigma: Why EMS Mental Health Isn’t Prioritized
Despite overwhelming evidence, barriers to seeking help persist:
“If I admit I’m struggling, I’ll lose my job.”
Fear of job loss, demotion, or judgment prevents providers from seeking care. Unlike physical injuries, mental health struggles are still perceived as weakness.
“I don’t have time for therapy. I barely have time to sleep.”
EMS schedules are brutal—48-hour shifts, mandatory overtime, and chronic exhaustion make consistent mental healthcare nearly impossible.
“It’s just part of the job.”
The “tough-it-out” culture in EMS tells providers to suppress emotions and keep moving. But unprocessed trauma doesn’t disappear, it accumulates until it becomes unmanageable.
Ignoring mental health doesn’t make EMS providers stronger—it makes them vulnerable.
Solutions: How EMS Can Take Mental Health Seriously
Systemic changes are necessary to prevent burnout, PTSD and suicide in EMS.
- Normalizing Mental Health Conversations in EMS
- Leadership must actively encourage open discussions about mental health.
- Senior providers should share their own experiences to reduce stigma.
- Mandatory Mental Health Check-Ins
- Annual mental health screenings should be as standard as physical checkups.
- Access to mental health professionals should not require a self-initiated request.
- Accessible & Confidential Support Services
- Peer support programs should be integrated into EMS agencies.
- Anonymous mental health resources (text-based counseling, crisis hotlines) should be readily available.
- Adjusting EMS Schedules for Mental Wellness
- Reducing back-to-back shifts to allow for recovery time.
- Implementing mental health leave options without job security concerns.
- Teaching Resilience and Coping Skills Early
- EMS education should include mandatory training on stress management and PTSD recognition.
- New EMTs and paramedics should be trained to recognize signs of burnout before they hit crisis levels.
Conclusion: It’s Time to Prioritize EMS Mental Health
Mental health in EMS is not a personal failure, it is a systemic issue that requires real change.
Until mental health is prioritized at the same level as trauma care, EMS will continue to see burnout, PTSD, and preventable suicides.
If we truly want to protect our patients, our partners, and ourselves, we must take EMS mental health seriously starting now.
 https://standingabovethecrowd.com/james-donaldson-on-mental-health-the-silent-struggle-addressing-the-mental-health-epidemic-in-ems/
https://standingabovethecrowd.com/james-donaldson-on-mental-health-the-silent-struggle-addressing-the-mental-health-epidemic-in-ems/