Physicians often fail to treat men’s mental health issues effectively. Better training and empathy for the distinct symptoms and societal expectations men face can help
By Derek M. Griffith, PhD, Ayo Ogunbiyi, MPH, and Emily Jaeger, MPH
Editor’s note: The opinions expressed by the authors do not necessarily reflect the opinions of the AAMC or its members.
Men in the United States die by suicide at a rate four times higher than women. And yet, men are diagnosed with depression and mood disorders at far lower rates. Why is this?
Too often, society blames men themselves for their struggles. They are the ones who often turn to substance abuse and violent behavior rather than getting help for their mental health. They are the ones who struggle to keep up with a changing workforce and gender norms. They are the ones who too often embrace unhealthy attitudes and beliefs at the expense of their own well-being.
But this approach of placing blame on individuals has produced little by way of clinical, social, or structural interventions to improve men’s mental health.
Men aren’t the problem. The way that we — society as a whole and health care providers specifically — treat them is.
It is time that primary care physicians, mental health service providers, and policymakers look critically at the accuracy and utility of their assumptions and explanations for men’s rates of depression, anxiety, burnout, substance abuse, and other common mental health conditions. The current framework has limited our ability to offer real solutions that meet men where they are and give them the tools to not only survive, but to thrive.
Unfortunately, in the United States, men’s health and well-being has reached a critical point. The COVID-19 pandemic exacerbated the crisis of men's mental health. Studies found that during the pandemic, U.S. men reported slightly lower rates of anxiety than women, but had higher rates of depressive symptoms and suicidal ideation than their female counterparts.
The uncertainty of the pandemic, loneliness from social distancing, financial stresses, relationship challenges, and other contextual factors contributed to increased rates of men having difficulty sleeping, alcohol and substance use, and post-traumatic stress disorder (PTSD) symptoms triggered by the experience of mechanical ventilation treatment and hospitalization. Consequently, at one point in 2020, the rates of men seeking mental health care services in the United States increased more than five-fold over the prior year. These rates were greater than the rates of women seeking mental health care services during this time. Yet, by 2021, just 40% of men with a reported mental illness received mental health care services in the past year, compared with 52% of women with a reported mental illness, according to the National Institute of Mental Health.
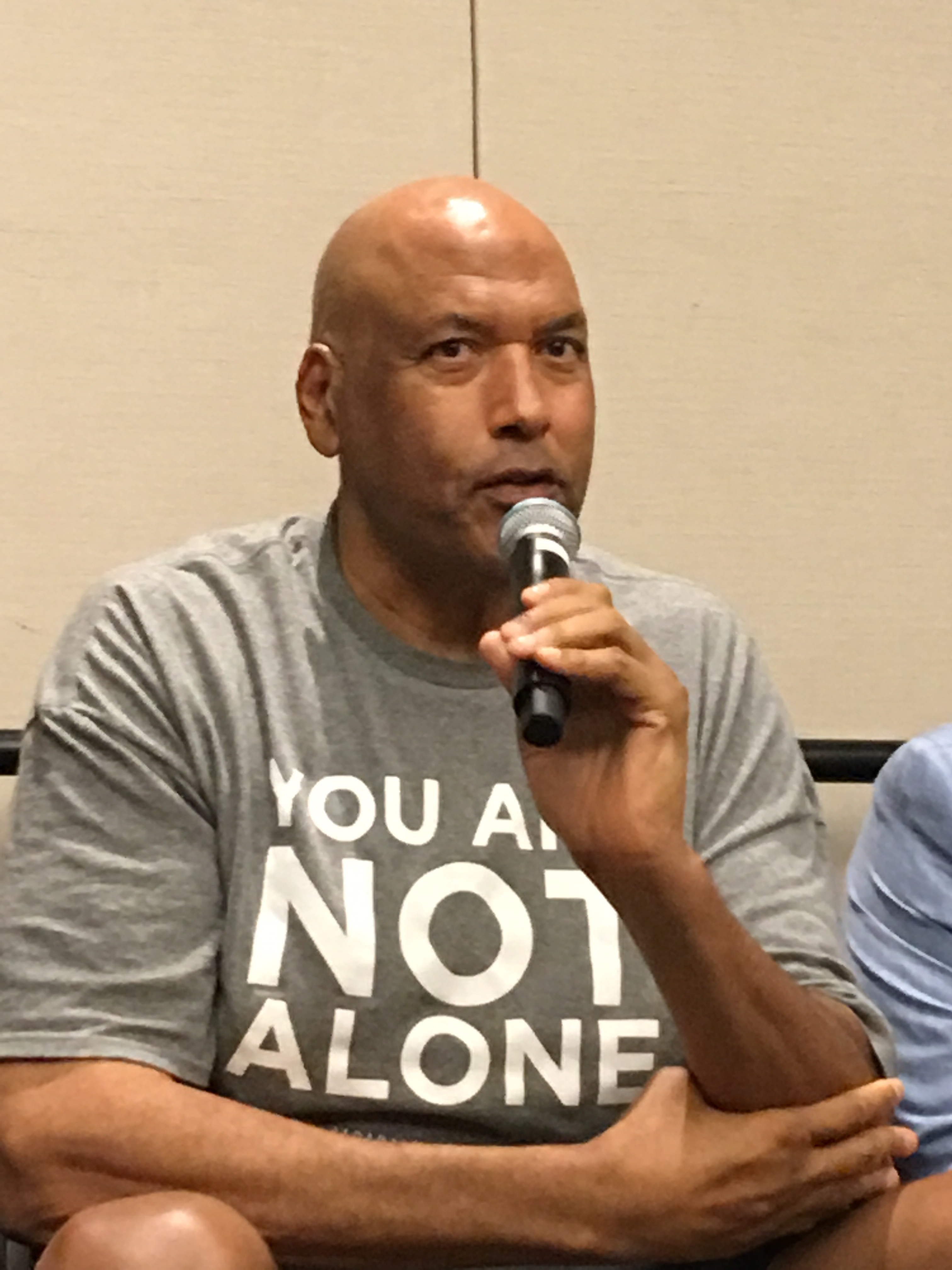
#James Donaldson notes:
Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.
Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.
Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticle
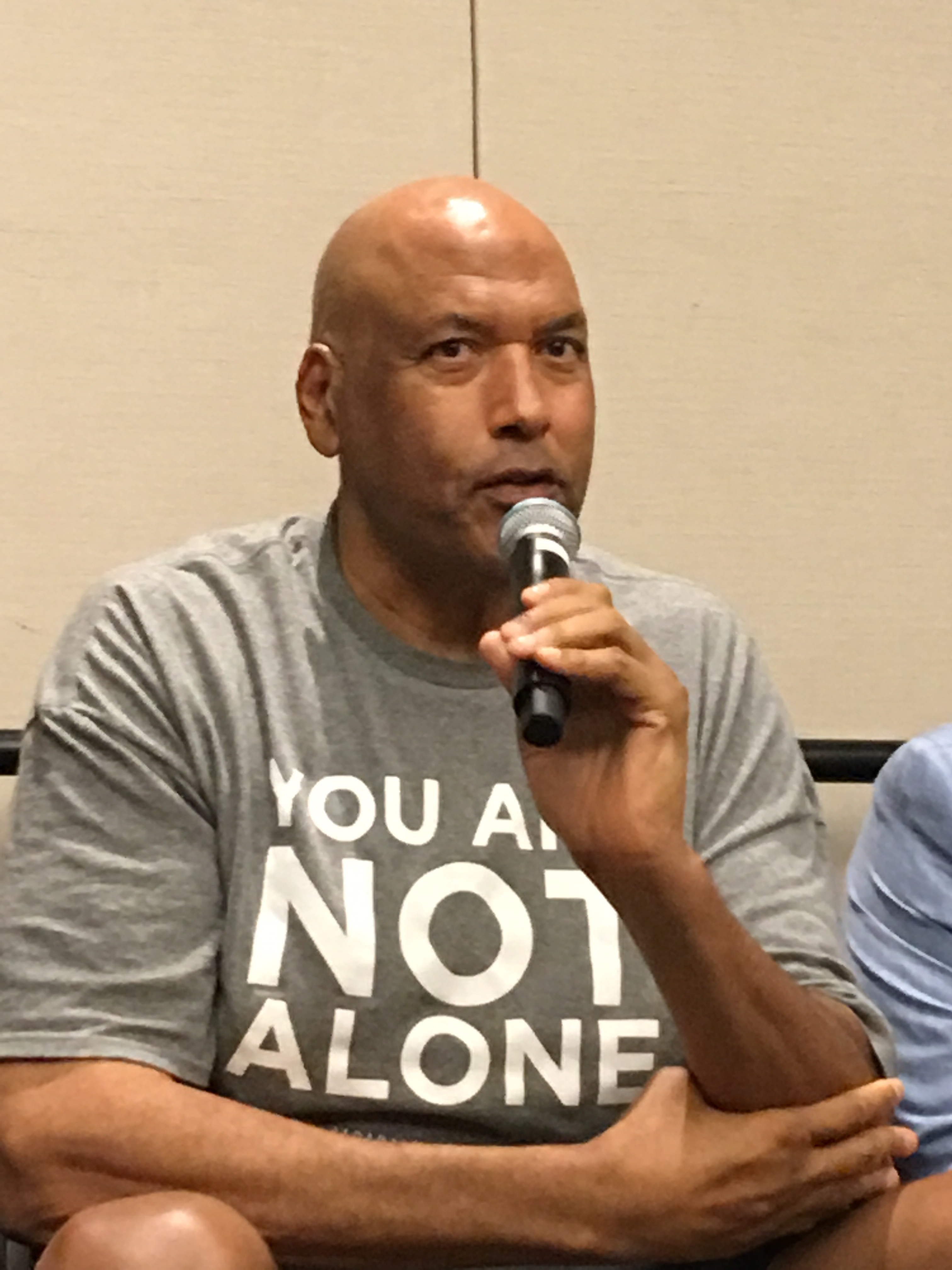
Find out more about the work I do on my 501c3 non-profit foundation
website www.yourgiftoflife.org Order your copy of James Donaldson's latest book,
#CelebratingYourGiftofLife: From The Verge of Suicide to a Life of Purpose and Joy
www.celebratingyourgiftoflife.com
Link for 40 Habits Signup
bit.ly/40HabitsofMentalHealth
If you'd like to follow and receive my daily blog in to your inbox, just click on it with Follow It. Here's the link https://follow.it/james-donaldson-s-standing-above-the-crowd-s-blog-a-view-from-above-on-things-that-make-the-world-go-round?action=followPub
Even when men seek care, that care often falls short. Data from Canada and the United States found that more than 60% of men who died by suicide had accessed mental health care services within the previous year. When men do seek mental health care services, it is not uncommon for them to feel that providers mislabel and underestimate their needs, and that these providers do not seem to have a genuine interest in their problems. For some time, research has shown that mental health providers may miss or misdiagnose psychological problems in men because of their own gender biases. They might believe that men simply need to “man up” and stop showing weakness, or that the symptoms they present are not consistent with diagnostic tools. Mental health providers may not consider that these tools do not take into account gender differences in experience or symptoms that men are more likely to exhibit.
For men to seek mental health care in the first place is already a challenge, with social barriers such as societal stigma, fear of judgment, and lack of skills to communicate emotions keeping many from doing so. It’s unconscionable that bias and a lack of effective treatment approaches on the part of mental health providers would create even more barriers. Men do bear a responsibility to seek help, but it’s far from illogical when they choose to avoid it.
The impetus is on those of us in the medical and mental health fields to ensure we’re empathetic to the struggles that men face in a changing world. Research has shown that men often struggle to differentiate depression from stress, and to know when to seek help if symptoms are severe enough. Men (and health care providers) may not label men’s symptoms as depression if the symptoms are tied to an external factor like unemployment. Traditionally, men are socialized to define their worth by their ability to contribute economically to a household. However, as the labor market has shifted away from traditionally male-dominated jobs, men must now redefine their worth outside of their employment, income, and home. The notion of "precarious manhood,” which is the belief that manhood is an achieved social status that must be earned and constantly defended, means that men may feel it is their character — rather than their behavior — being judged during more tumultuous economic times.
Even men who do achieve and maintain a certain level of manhood they perceive as successful are likely to put unreasonable expectations on themselves that can lead to burnout. An imbalance between job demands and job skills, lack of control over tasks at work, lack of reward or acknowledgement of effort, and prolonged work stress are some of the leading factors contributing to burnout. As we think about the ways gender influences how men present with mental health symptoms, it is important to keep these contextual factors in mind.
The fact that men are diagnosed with depression at lower rates than women, despite their higher rates of suicide, substance use, and violent behavior, suggests that more could be done to improve the tools used to diagnose men with depression. Several scholars have noted the importance of increasing the capacity of mental health care service providers’ ability to consider gender in the presentation of mood disorders among men. While some mental health care service providers may be gender sensitive and recognize the ways that aggressiveness, alcohol use, and risky behavior are part of the presenting symptoms men with depression may exhibit, there are few courses and trainings that focus on gender differences in mental health, potentially leading to mental health care service providers being less equipped to serve and offer gender-sensitive resources to men.
Given the data and the unique contexts and aspects of men’s mental health, there is a need to create more opportunities for health care providers who serve men to learn to be sensitive and responsive to their male patients’ needs. Along with efforts like the Movember Foundation's Rooted and Rising Collective and the Canadian Men’s Health Foundation MindFit Toolkit, Table 1 below highlights selected programs and e-health tools that have been designed to be sensitive to the presentation, needs, and preferences of men. These resources demonstrate examples of gender-sensitive interventions to promote men’s mental health. Part of what makes these programs successful is that they recognize that men are not a monolith, and that it is critical to develop culturally sensitive interventions that consider the ways groups of men are unique.
The reasons men may need mental health resources and support are not simply due to how men think, or because of their attitudes about masculinity. Using a lens this narrow hampers our capacity to effectively address and improve men’s health. It is important to consider the gender sensitivity of mental health services, and the broader contextual and structural factors that influence men’s mental health and well-being. It is time we consider men’s mental health in its full context, and shift the focus to the ways our health care systems and providers are equipped to deliver services to improve men’s mental health.
https://standingabovethecrowd.com/james-donaldson-on-mental-health-men-and-mental-health-what-are-we-missing/


No comments:
Post a Comment