By Kelly Wairimu Davis, MS
How should the #media safely report on #suicide?
The news of #MissUSA2019 #CheslieKryst’s untimely death by #suicide on Jan. 30 stunned the world. Scrolling through breaking news headlines and #socialmedia feeds, many questioned how an accomplished lawyer, TV host, and social activist could have taken her own life at age 30.
Comments expressing condolences and well wishes to her family and friends poured in, along with reminders to always check in on friends and family members.
But for a certain group of people, headlines and #socialmedia posts with graphic details about Kryst’s death stirred up feelings of #hopelessness and despair of their own.
“While most people will ingest these things without having any kind of problem in relation to it, some small group of vulnerable people might be impacted in ways that are dangerous, even leading to #suicide contagion,” says Victor Schwartz, MD, a clinical associate professor of psychiatry at New York University #School of Medicine.
Finding Support When You Have #TreatmentResistantDepression
Share Share on #Facebook Share on #Twitter Share on #Pinterest
1 / 12When #Depression Resists Treatment It's hard not to feel hopeless when #depression treatment doesn't work. But don't give up. As many as two-thirds of people with #depression aren't helped by the first antidepressant they try. Work with your #doctor to find the best treatments. #Depression is highly treatable, and there are many options available. You might find that changing your medication, combining drugs, seeing a specialist, or talking to a #therapist helps your recovery and reduces relapses.
2 / 12Talk Therapy for Focus and Insight Talking with a #mentalhealthprofessional can help you set goals, tackle problems, and stay focused on medical treatment for your #depression. Talk therapy is an important part of treatment for many people with chronic and #treatmentresistantdepression (#TRD). Ask your #doctor to help you find a #therapist whom you can work with effectively. Talk therapy includes individual psychotherapy and support groups.
3 / 12Therapy That Can Help Some people may benefit from specific types of therapy. #Cognitivebehavioraltherapy (#CBT) attempts to break down ineffective or destructive patterns of thinking that may contribute to #depression. Problem-solving therapy, a type of #CBT, may help people with #depression cope with negative or stressful life experiences. Interpersonal psychotherapy examines issues like grief, which may affect the relationships between people or cause #depression.
4 / 12Find the Right Medications Many people who start taking an antidepressant don’t have a complete recovery and may need a change in treatment. You should see some improvement after six weeks. If your antidepressant isn't working, your #doctor may change your prescription or increase your dosage, or prescribe other antidepressants or even other types of drugs to go with it. Continue to take it as prescribed, even if you start to feel better.
5 / 12Which Antidepressant Is Right? The most commonly prescribed antidepressants, known as SSRIs and SNRIs, affect the brain chemicals serotonin or both serotonin and norepinephrine, respectively. Your #doctor considers side effects, safety, tolerability, and your history of #depression when prescribing antidepressants. You may experience mild to severe side effects like dry mouth, nausea, #insomnia, sexual problems, changes in blood pressure, or suicidal thoughts from antidepressants. Sometimes side effects go away. If severe side effects persist, talk to your #doctor about changing medicines.
6 / 12Other Treatments for #Depression If several courses of different antidepressants have failed, you and your #doctor might consider other medical treatments that can help treatment-resistant #depression. Electroconvulsive therapy uses small electric currents to cause a brief seizure in the brain. Transcranial magnetic stimulation (shown) sends magnetic pulses to the brain to improve mood.
7 / 12Pastoral and Spiritual Counseling Make sure you have enough support from family and friends so you can cope with your #depression. Many people find comfort from being part of a spiritual community. If you are religious, talk with your priest, rabbi, minister, or other religious advisor. These people often know you and your family as individuals. And they can help you articulate the things that are important to you. They'll also help you understand your role in the community.
8 / 12Volunteer for a Sense of Worth #Depression feeds on #isolation. When you separate yourself from the community, your sense of having no value grows stronger. Volunteering is a perfect antidote. It gives you something to do and turns your focus outside yourself. At the same time, it makes you feel good about who you are. Find something you value. Then offer to help.
9 / 12Let Your Family Help #Depression is hard on you and your family. But remember, they can't help if you won't let them. If you share your feelings, you won't create a divide between you and those you love. Let them help when they can, and consider couples or family counseling. Let your family know they are important in your life.
10 / 12Plan to Feel Better You don't always do things that make you happy. But planning enjoyable activities for each day can help your treatment. Each afternoon, jot down a list of what you want to do for yourself the next day. Then add what you need to do for others. Review your plan at the end of each day. How did the things you accomplished make you feel?
11 / 12Exercise, a Natural Medicine You may not feel like exercising. But exercise is effective in easing #depression. Your body's physical response to exercise actually improves your mood. That's because exercise causes the release of endorphins. These chemicals trigger a positive feeling. It doesn't matter what kind of exercise you do. Just find something you enjoy and start moving.
12 / 12Support From Others Who Understand A support group is made up of people who know what it feels like to be depressed. It helps to know others understand how you feel. Even more important, they can share coping techniques from their own experience. Plus you have the opportunity to share your successes with them. Ask your #doctor to help you find a support group in your area.
Reviewed by Neha Pathak
#Suicidecontagion is “the process by which one or more suicides increase the risk of #suicidalbehavior in others,” according to the #AmericanAssociationofSuicidology.
#Media coverage of a death by #suicide plays a critical role in vulnerable people’s safety after such news, says Madelyn S. Gould, PhD, a professor of psychiatry at Columbia University Irving Medical Center in New York.
“There’s been a myriad of research in this area, and it’s clear that there’s a real impact of the #media on subsequent suicides, depending on how the story is shaped, how headlines are shaped, and the pictures that are included in the article,” she says. “It could be the difference between life and death for a vulnerable person who gets triggered by the way the story was written.” And news of celebrity suicides can lead to particularly harmful outcomes, Gould says.
“They may have been identifying with that celebrity for years or envision a perfect life. ‘How could that person be vulnerable to #suicide?’” she says. “For another vulnerable person, it can make them feel even more hopeless about the situation.”
Shaping the story to offer hope to those who may be struggling with #suicidalthoughts, as well as sharing helpful resources, can make a huge difference, #suicideprevention experts say.
“Is it a story about hope and healing and encouraging health coping strategies, or is it glorification of someone’s death by #suicide?” Gould says.
“If the story presents #suicide as a ‘coping mechanism,’ then the greater number of those types of stories, unfortunately, the greater likelihood that there will be subsequent deaths by #suicide.”
WebMD spoke to #suicideprevention experts who analyzed #media outlets’ coverage of Kryst’s death. Read on for a look at how they say safe reporting practices could save lives.
How to Report on #Suicide
Many #suicideprevention organizations -- such as the #AmericanFoundationforSuicidePrevention, #AmericanAssociationofSuicidology, and #WorldHealthOrganization -- have published guidelines on safe reporting strategies.
One of the most universal principles is not reporting the method by which the #suicide took place.
Information about location and time, and other sensitive material, like photos, videos, or mention of #suicide notes, should also be largely avoided.
“Things like method or very graphic details about someone’s death from #suicide can have a tendency to provide a way for people to identify with that death,” says Chris Maxwell, director of public relations and #media at the #AmericanAssociationofSuicidology.
It’s also important to steer clear of overly emotional or dramatic language when reporting on deaths by #suicide, which can run counter to certain aspects of journalism, says Schwartz.
“The fundamental problem with reporting on celebrity #suicide is that if you look at the guidelines for safe reporting, they’re almost exactly the opposite of what journalists are typically trained to do,” he says. “We’re trying to have it not be incendiary, exciting, interesting, or romantic.” The experts help us analyze different outlets’ headlines and reporting of Kryst’s death to better understand how #media can cover #suicide safely and effectively.
#James Donaldson notes:Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticleOrder your copy of James Donaldson's latest book,#CelebratingYourGiftofLife:From The Verge of Suicide to a Life of Purpose and Joy
http://www.celebratingyourgiftoflife.com
#Media Coverage of #CheslieKryst’s Death
The New York Times
“That’s fairly objective,” Maxwell says. “At least in the headline or the subheading, there’s not necessarily a method. #Suicide isn’t directly mentioned.”
“In mentioning #suicide in general, we have to have a balance. It’s OK to say someone dies by #suicide without necessarily talking about a method.”
Fox News
“They immediately say she jumped to her death and tell us from where, and then describe the building, so they are describing the actual #suicide and the means to #suicide,” Schwartz says.
“Journalists are walking a kind of tightrope here, because if you present this like it’s a clinical research paper, people could accuse you of being heartless. But you don’t have to open up the article with describing how she jumped from the 29th floor of a particular building and what time.”
New York Post
“I would absolutely not include anything about jumping from a high-rise,” Maxwell says. “It’s outside of any sort of guidelines or recommendations.”
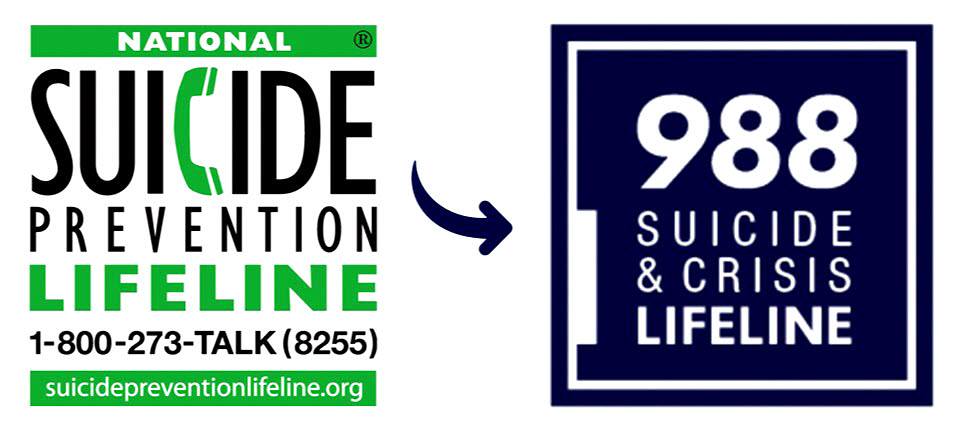
“These pictures are totally irresponsible, with no opportunity to be talking about treatment for #depression or calling the #NationalSuicidePreventionLifeline -- which will soon be accessed by calling, chatting or texting 988 -- folks can call, chat, or text if they are worried about someone else or if they are suicidal themselves,” Gould says.
NBC News
“’Her body was found in a Manhattan neighborhood near Times Square’ -- that’s an interesting way to phrase it,” says Maxwell.
“I can’t imagine that adding anything to the story. Saying that she died, and that she accomplished all these things, seems much more core to the story and much more effective at talking about who she was. That’s what we should be focusing on.”
Social Media Considerations
#Socialmedia posts about deaths by #suicide can be tricky, since these platforms also serve as a space for healing and unity between those who have been affected by #suicide, says Dimple Patel, PsyD, a therapist and board member of the #AmericanFoundationforSuicidePrevention’s Illinois chapter.
“I’ve met so many people on #Instagram, #TikTok, and #Facebook who I’ve connected through shared experience of losing someone or being in that grief process,” says Patel, who lost her mother to #suicide in 2011.
“There is a form of community there for those who are struggling. They can connect with people who are feeling the same way.”
But problems can also arise, especially if posts aren’t closely monitored, which ultimately reflects the “pros and cons of #socialmedia,” says Aneri Pattani, a Kaiser Health News reporter and 2021 Bloomberg fellow at Johns Hopkins Bloomberg School of Public Health.
“You have the ability to talk about an issue that is often stigmatized and that is not talked about, which can also be detrimental,” Pattani says. “So, in some ways, that’s great that it brings the conversation forward like that and to people on a platform where they might be more comfortable engaging with it.”
“At the same time, you have no idea when you put something on #socialmedia who it’s going to reach and what state they’re going to be in.”
One potential way to promote safety for vulnerable people could be using “trigger warnings” in posts about #suicide, along with including information on resources like the #NationalSuicidePreventionLifeline and the Crisis Text Line.
“As someone is seeing your story or call out, if they are in a vulnerable position, they are also finding the resources right there and then,” Pattani says.
Joining Forces
Having advocates within journalism promoting safe reporting practices through training and dialogue with colleagues can be a big part of bringing about change, says Gould.
And some journalists in the field have already begun this work.
Pattani and Holly Wilcox, PhD, a professor at the Johns Hopkins Bloomberg School of Public Health, are joining forces with Johns Hopkins and the Bloomberg American Health Initiative to create a free course for journalists that teaches responsible reporting practices.
Myths and Facts About #Depression
Share Share on #Facebook Share on #Twitter Share on #Pinterest
1 / 18Myth: Hard Work Beats #Depression #Depression affects nearly one in six people at some point in their lives, so folk remedies and half-truths about this common illness abound. One such idea: throw yourself into work and you'll feel better. For a mild case of the blues, this may indeed help, but #depression is a different animal. Overworking can actually be a sign of clinical #depression, especially in men.
2 / 18Myth: It's Not a Real Illness #Depression is a serious medical condition -- and the top cause of disability in #American #adults. But it's still confused with ordinary sadness. Biological evidence of the illness comes from studies of genetics, hormones, nerve cell receptors, and brain functioning. Nerve circuits in brain areas that regulate mood appear to function abnormally in #depression.
3 / 18Fact: #Men Fly Under the Radar A depressed #man, their loved ones, and even their #doctor may not recognize #depression. That's because #men are less likely than #women to talk about their feelings -- and some depressed #men don't appear sad or down. Instead, #men may be irritable, angry, or restless. They may even lash out at others. Some men try to cope with #depression through reckless #behavior, drinking, or drugs.
4 / 18Myth: #Depression Is Just #Self-Pity Our culture admires will power and mental toughness and is quick to label anyone who falls back as a whiner. But people who have clinical #depression are not lazy or simply feeling sorry for themselves. Nor can they "will" #depression to go away. #Depression is a medical illness -- a health problem related to changes in the brain. Like other illnesses, it usually improves with appropriate treatment.
5 / 18Fact: Anyone Can Get Depressed Poet or linebacker, shy or outgoing, anyone from any ethnic background can develop #depression. The illness is twice as common in #women as in #men, but it may be that women are more likely to seek help. It's often first noticed in the late #teens or 20s, but an episode can develop at any age. Tough personal experiences can sometimes trigger #depression in people who are at risk for the illness. Or it may develop out of the blue.
6 / 18Fact: It Can Sneak Up Slowly #Depression can creep up gradually, which makes it harder to identify than a sudden illness. A bad day turns into a rut and you start skipping work, #school, or social occasions. One type, called dysthymia, can last for years as a chronic, low-level illness – a malaise that silently undermines your career and relationships. Or #depression can become a severe, disabling condition. With treatment, many feel substantial relief in 4-6 weeks.
7 / 18Myth: Help Means Drugs for Life Despite the buzz about a "Prozac Nation," medication is only one of the tools used to lift #depression. Asking for help doesn't necessarily mean your #doctor will advise medications, although medicines can often be very helpful for significant forms of depression. Studies suggest, though, that "talk" therapy works as well as drugs for mild to moderate #depression. Even if you do use antidepressants, it probably won’t be for life. Your #doctor will help you determine the right time to stop your medication.
8 / 18Myth: Depressed People Cry a Lot Not always. Some people don't cry or even act terribly sad when they're depressed. Instead they may appear emotionally "blank" and may feel worthless or useless. Even without dramatic symptoms, untreated #depression prevents people from living life to its fullest -- and takes a toll on families.
9 / 18Fact: Family History Is Not Destiny If #depression appears in your family tree, you're more likely to experience it, too. But chances are you won't. People with a family history can watch for early symptoms of #depression and take positive action promptly -- whether that means reducing #stress, getting more exercise, counseling, or other professional treatment.
10 / 18Myth: #Depression Is Part of Aging Most people navigate the challenges of aging without becoming depressed. But when it does occur, it may be overlooked. Older people may hide their sadness or have different, vague symptoms: food just doesn't taste good anymore, aches and pains worsen, or sleep patterns change. Medical problems can trigger #depression in seniors -- and #depression can slow recovery from a heart attack or surgery.
11 / 18Fact: #Depression Imitates #Dementia In #seniors, #depression can be the root cause of memory problems, confusion, and in some cases, delusions. #Caregivers and #doctors may mistake these problems for signs of #dementia, or an age-related decline in memory. Getting treatment lifts the cloud for the majority of older people with #depression. Psychotherapy can also be a useful part of treatment for older #adults with #depression who may be coping with loss, medical illnesses, or other life changes.
12 / 18Myth: Talking Makes Things Worse People were once advised not to "dwell on" problems by talking about them. Today, there's evidence that guided discussions with a professional can make things much better. Different types of psychotherapy help treat #depression by addressing negative thought patterns, unconscious feelings, or relationship troubles. The first step is to talk to a #mentalhealthprofessional.
https://standingabovethecrowd.com/?p=10019


No comments:
Post a Comment